User:MdWikiBot/Vasectomy
| Vasectomy | |
|---|---|
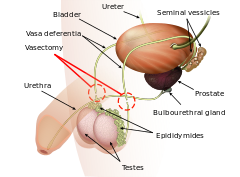 Diagram of the anatomy of a vasectomy | |
| Background | |
| Synonyms | Vasoligation; male sterilization |
| Type | Sterilization |
| First use | 1899[1] |
| Failure rates (first year) | |
| Perfect use | 0.10%[2] |
| Typical use | 0.15%[2] |
| Usage | |
| Duration effect | Permanent[3] |
| Reversibility | Occasionally[3] |
| User reminders | Semen analysis at 3 months to confirm effectiveness[3] |
| Advantages and disadvantages | |
| STI protection | None[4] |
| Benefits | Only requires injectable freezing.[3] Lower cost and safer than tubal ligation.[5][4] |
| Risks | Hematoma, infection, long-term pain[3] |
Vasectomy is a surgical procedure for sterilization of males.[3] At least 3 month and 20 ejaculations are generally required for effectiveness, which should be confirmed by semen analysis.[3] Failure rates at this point are about 1 in 2,000.[3] It is generally a permanent method of birth control; though, reversal methods include vasectomy reversal and sperm retrieval with in vitro fertilization.[3]
While generally safe, side effects in 1 to 2% may include hematoma or infection.[3] Postvasectomy pain syndrome may occur in up to 6%.[3] It does not alter sexual function.[4] It generally involves removing a piece of each vas deferens and sealing the ends which prevents sperm from entering the penis and thereby preventing fertilization.[3]
The procedure is often carried out in a warm doctor's office.[3][4] Numbing cream may be applied before injectable freezing.[3] Hair is removed and the area cleaned.[3] The vas deferens is brough near the skin at a point halfway between the testicle and penis.[3] To reach the vas the overlying skin may be cut with a scalpel or opened with dissecting forceps in the no-scalpel technique.[3] A segment of vas is than removed with the remaining ends clipped or tied closed and cauterized.[3] Paracetamol (acetaminophen) and NSAIDs may be taken for pain.[3] Heavy lifting and sex are not recommended for a week afterwards.[3][4]
The procedure was first performed in 1899 by Reginald Harrison.[1][6] As of 2020, it is used by 17 million reproductive aged women (1.8%) as a method of birth control.[7] This is a decrease from 6% in 1995.[7] In the United States the procedure generally costs less than 1,000 USD as of 2021;[3] which is less expensive than tubal ligation.[5]
References
change- ↑ 1.0 1.1 Newton, David E. (2 December 2019). Birth Control: A Reference Handbook. Bloomsbury Publishing USA. p. PT148. ISBN 979-8-216-05405-4. Archived from the original on 28 March 2024. Retrieved 25 March 2024.
- ↑ 2.0 2.1 Trussell, James (2011). "Contraceptive efficacy". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. Table 26–1 = Table 3–2 Percentage of women experiencing an unintended pregnancy during the first year of typical use and the first year of perfect use of contraception, and the percentage continuing use at the end of the first year. United States.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 Zeitler, M; Rayala, B (December 2021). "Outpatient Vasectomy: Safe, Reliable, and Cost-effective". Primary care. 48 (4): 613–625. doi:10.1016/j.pop.2021.08.001. PMID 34752273.
- ↑ 4.0 4.1 4.2 4.3 4.4 Fainberg, J; Kashanian, JA (19 June 2018). "Vasectomy". JAMA. 319 (23): 2450. doi:10.1001/jama.2018.6514. PMID 29922830.
- ↑ 5.0 5.1 Stormont, G; Deibert, CM (January 2024). "Vasectomy". StatPearls. PMID 31751094.
- ↑ Ciment, James (4 March 2015). Social Issues in America: An Encyclopedia. Routledge. p. 4. ISBN 978-1-317-45971-2. Archived from the original on 28 March 2024. Retrieved 25 March 2024.
- ↑ 7.0 7.1 World Family Planning 2022 (PDF). United Nations. 2022. ISBN 9789211483765. Archived (PDF) from the original on 7 December 2023. Retrieved 22 March 2024.