User:Mr. Ibrahem/Oxycodone
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | ɒksɪˈkəʊdəʊn |
| Trade names | OxyContin, others |
| Synonyms | Eukodal, eucodal; dihydrohydroxycodeinone, 7,8-dihydro-14-hydroxycodeinone, 6-deoxy-7,8-dihydro-14-hydroxy-3-O-methyl-6-oxomorphine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682132 |
| License data | |
| Pregnancy category |
|
| Dependence liability | High[1] |
| Routes of administration | By mouth, sublingual, intramuscular, intravenous, intranasal, subcutaneous, transdermal, rectal, epidural |
| Drug class | Opioid[3] |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | By mouth: 60–87%[4] |
| Protein binding | 45%[4] |
| Metabolism | Liver: mainly CYP3A, and, to a much lesser extent, CYP2D6 (~5%);[4] 95% metabolized (i.e., 5% excreted unchanged) |
| Metabolites | • Noroxycodone (25%) [5] • Noroxymorphone (15%, free and conjugated)[5] • Oxymorphone (11%, conjugated)[5] • Others (e.g., minor metabolites) |
| Onset of action | IR: 10–30 minutes CR: 1 hour[6] |
| Elimination half-life | By mouth (IR): 2–3 hrs (same t1/2 for all ROAs) By mouth (CR): 4.5 hrs |
| Duration of action | By mouth (IR): 3–6 hrs By mouth (CR): 10–12 hrs |
| Excretion | Urine (83%)[4] |
| Identifiers | |
| |
| Chemical and physical data | |
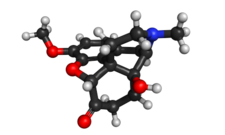
| Formula | C18H21NO4 |
| Molar mass | 315.37 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 219 °C (426 °F) |
| Solubility in water | HCl: 166 |
| |
| |
| (verify) | |
Oxycodone, sold under the brand name OxyContin among others, is an opioid medication used for treatment of moderate to severe pain.[3] It is usually taken by mouth, and is available in immediate-release and controlled-release formulations.[3] Onset of pain relief typically begins within 15 minutes and lasts for up to six hours with the immediate-release formulation.[3] In the United Kingdom, it is available by injection.[8] Combination products are also available with paracetamol (acetaminophen), ibuprofen, naloxone, and aspirin.[3]
Common side effects include constipation, nausea, sleepiness, dizziness, itching, dry mouth, and sweating.[3] Severe side effects may include addiction, respiratory depression (a reduction in breathing), and low blood pressure.[3] Those allergic to codeine may also be allergic to oxycodone.[3] Use of oxycodone in early pregnancy appears relatively safe.[3] Opioid withdrawal may occur if rapidly stopped.[3] Oxycodone acts by activating the μ-opioid receptor.[9] When taken by mouth, it has roughly 1.5 times the effect of the equivalent amount of morphine.[10]
Oxycodone was first made in Germany in 1916 from thebaine.[11] It is on the World Health Organization's List of Essential Medicines as an alternative to morphine.[12] It is available as a generic medication.[3] In the United States, the wholesale cost per dose is less than US$0.30 as of 2018.[13] In 2017, it was the 52nd most commonly prescribed medication in the United States, with more than 15 million prescriptions.[14][15] Oxycodone has been a common drug of abuse.[16] A number of abuse-deterrent formulations are available, such as in combination with naloxone.[16][17]
References
change- ↑ Bonewit-West, Kathy; Hunt, Sue A.; Applegate, Edith (2012). Today's Medical Assistant: Clinical and Administrative Procedures. Elsevier Health Sciences. p. 571. ISBN 9781455701506. Archived from the original on 2020-07-28. Retrieved 2020-08-05.
- ↑ 2.0 2.1 "Oxycodone Use During Pregnancy". Drugs.com. 14 October 2019. Archived from the original on 19 June 2020. Retrieved 12 April 2020.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 "Oxycodone Monograph for Professionals". Drugs.com. AHFS. Archived from the original on 28 December 2018. Retrieved 28 December 2018.
- ↑ 4.0 4.1 4.2 4.3 "Roxicodone, OxyContin (oxycodone) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 13 April 2014. Retrieved 8 April 2014.
- ↑ 5.0 5.1 5.2 "Roxicodone, OxyContin (oxycodone) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 13 April 2014. Retrieved 4 January 2019.
- ↑ Connie Henke Yarbro; Debra Wujcik; Barbara Holmes Gobel (15 November 2010). Cancer Nursing: Principles and Practice. Jones & Bartlett Publishers. pp. 695–. ISBN 978-1-4496-1829-2. Archived from the original on 27 February 2020. Retrieved 5 August 2020.
- ↑ "Interpreting Urine Drug Tests (UDT)". Archived from the original on 25 October 2023. Retrieved 24 October 2023.
- ↑ British national formulary : BNF 74 (74 ed.). British Medical Association. 2017. p. 442. ISBN 978-0857112989.
- ↑ Nicholas J Talley; Brad Frankum; David Currow (10 February 2015). Essentials of Internal Medicine 3e. Elsevier Health Sciences. pp. 491–. ISBN 978-0-7295-8081-6. Archived from the original on 3 August 2020. Retrieved 5 August 2020.
- ↑ "Stanford School of Medicine, Palliative Care, Opioid Conversion / Equivalency Table". 2013-04-20. Archived from the original on 2020-09-09. Retrieved 2020-08-05.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Sneader, W. (2005). Drug discovery: a history. Hoboken, NJ: Wiley. p. 119. ISBN 978-0-471-89980-8.
- ↑ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ↑ "NADAC as of 2018-12-19". Centers for Medicare and Medicaid Services. Archived from the original on 2018-12-19. Retrieved 22 December 2018.
- ↑ "The Top 300 of 2020". ClinCalc. Archived from the original on 12 February 2021. Retrieved 11 April 2020.
- ↑ "Oxycodone - Drug Usage Statistics". ClinCalc. Archived from the original on 11 April 2020. Retrieved 11 April 2020.
- ↑ 16.0 16.1 Pergolizzi JV, Jr; Taylor R, Jr; LeQuang, JA; Raffa, RB (2018). "Managing severe pain and abuse potential: the potential impact of a new abuse-deterrent formulation oxycodone/naltrexone extended-release product". Journal of Pain Research. 11: 301–311. doi:10.2147/JPR.S127602. PMC 5810535. PMID 29445297.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ Dart, RC; Iwanicki, JL; Dasgupta, N; Cicero, TJ; Schnoll, SH (2017). "Do abuse deterrent opioid formulations work?". Journal of Opioid Management. 13 (6): 365–378. doi:10.5055/jom.2017.0415. PMID 29308584.