Acinetobacter baumannii
Acinetobacter baumannii (A. baumannii) is a pathogenic bacterial species that causes disease in humans. It is commonly found in soil and water.[2] A. baumannii is the most important member of the Acinetobacter genus associated with infections gained in hospitals.[2] A.Baumannii is resistant to a specific class of antibiotic called carbapenems. Carbapenems-resistant Acinetobacter infection is common in hospitals and is very dangerous.[2] In 2017, it resulted in an estimated 8,500 infections in hospital patients and 700 deaths in the United States of America.[2] The World Health Organisation (WHO) released a list of top bacteria pathogens of concern, called ESKAPE pathogens, due to their high levels of antibiotic resistance.[3] A. baumannii was named as one of the most dangerous ESKAPE pathogens.[4] In order to treat A. baumannii effectively, it is important to understand how it acts as pathogen and its mechanism of antibiotic resistance.
| Acinetobacter baumannii | |
|---|---|
| |
| Acinetobacter baumannii | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Pseudomonadales |
| Family: | Moraxellaceae |
| Genus: | Acinetobacter |
| Species: | A. baumannii
|
| Binomial name | |
| Acinetobacter baumannii Bouvet and Grimont 1986[1]
| |
Biology
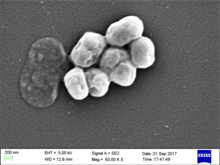
changeA. baumannii are short and rod-shaped. They average between 1.0 and 1.5 micrometers in length. They do not all look the same and can vary in size and shape.[5] Acinetobacter do not have a flagella, a tail-like structure used by many bacteria to move around. They are immobile but sometimes twitch and swarm to move around.
Habitat
changeThe first Acinetobacter was found in the soil by M.W. Beijerink in 1911.[6] Since then, it has also been found in water, animals, and humans.[6] A. baumannii are often found in hospitals and makeup almost 15% of infections that are transmitted in hospitals.[5] A. baumannii target moist environments. The respiratory tract, blood, open wounds, skin, and eyes are all possible sites of infection.[6]
Hospital infections
changeA. baumannii can cause many different diseases with different symptoms. Types of infection include pneumonia, bloodstream infections, meningitis, skin and bone infections and urinary tract infections.[7] The most common infections are pneumonia and bloodstream infections. Factors that increase the risk of infection include a weak immune system, long hospital stays, hospital ventilators and the tubes used on them, and having an open wound.[5]
It can be difficult to tell the difference between symptoms of A. baumannii infection and symptoms of other hospital infections. Symptoms include fever, rash, confusion, urinating pain, nausea, muscle and chest pains, breathing difficulties, and coughing.[8]
A. baumannii is spread through contact with contaminated surfaces, objects, and skin of contaminated patients. It can survive on surfaces for a long time before infecting new patients making it an effective pathogen.[9]
Treatment
changeCarbapenems are a type of antibiotics that have been used to treat Acinetobacter baumannii infections. These antibiotics are effective in treating infection. However, A. baumannii can develop tolerance to this antibiotic. This tolerance makes it harder to treat infections.[5] Carbapenems-resistant A. baumannii can spread their tolerance to other types of bacteria. This is dangerous in healthcare settings because if many bacteria are tolerant to carbapenems, the antibiotic cannot be used to treat infections anymore. A. baumannii can be tolerant to multiple antibiotics making infections difficult to treat.[10]
Polymyxins are another antibiotic used to treat A. baumannii infection.[11] These are effective against infection but polymyxins can be toxic to the kidneys.[12]
Combination therapies can also be used to treat A. baumannii which is tolerant to many different types of antibiotics. This means treating the infection with a combination of different drugs at the same time. Different combinations are still being tested against A. baumannii infections.[4]
Prevention of infection
changePreventing and controlling outbreaks of A. baumannii is very important. Preventing infections will reduce the number of infections in hospitals and help stop the spread of antibiotic resistance.
A. baumannii can be controlled with strict infection control measures such as educating hospital staff about the dangers of spreading hospital infections, proper hand washing, cleaning of hospitals and actively testing surfaces for the presence of A. baumannii[13]. These measures have been shown to reduce the spread of A. baumannii and reduce tolerance to antibiotics. However, all measures must be followed strictly to control infection.[13]
Related pages
changeReferences
change- ↑ Parte, A.C. "Acinetobacter". LPSN.
- ↑ 2.0 2.1 2.2 2.3 "Acinetobacter". CDC.
- ↑ Mulani, Mansura S.; Kamble, Ekta E.; Kumkar, Shital N.; Tawre, Madhumita S.; Pardesi, Karishma R. (2019-04-01). "Emerging Strategies to Combat ESKAPE Pathogens in the Era of Antimicrobial Resistance: A Review". Frontiers in Microbiology. 10: 539. doi:10.3389/fmicb.2019.00539. ISSN 1664-302X. PMC 6452778. PMID 30988669.
- ↑ 4.0 4.1 Lee, Chang-Ro; Lee, Jung Hun; Park, Moonhee; Park, Kwang Seung; Bae, Il Kwon; Kim, Young Bae; Cha, Chang-Jun; Jeong, Byeong Chul; Lee, Sang Hee (2017-03-13). "Biology of Acinetobacter baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and Prospective Treatment Options". Frontiers in Cellular and Infection Microbiology. 7: 55. doi:10.3389/fcimb.2017.00055. ISSN 2235-2988. PMC 5346588. PMID 28348979.
- ↑ 5.0 5.1 5.2 5.3 Asif, Muhammad; Alvi, Iqbal Ahmad; Rehman, Shafiq Ur (2018-08-21). "Insight into Acinetobacter baumannii: pathogenesis, global resistance, mechanisms of resistance, treatment options, and alternative modalities". Infection and Drug Resistance. 11: 1249–1260. doi:10.2147/IDR.S166750. PMC 6110297. PMID 30174448.
- ↑ 6.0 6.1 6.2 Howard, Aoife; O’Donoghue, Michael; Feeney, Audrey; Sleator, Roy D. (2012). "Acinetobacter baumannii: An emerging opportunistic pathogen". Virulence. 3 (3): 243–250. doi:10.4161/viru.19700. ISSN 2150-5594. PMC 3442836. PMID 22546906.
- ↑ Kanafani, Zeina A.; Kanj, Souha S. (2020). "Acinetobacter infection: Epidemiology, microbiology, pathogenesis, clinical features, and diagnosis". UpToDate.
- ↑ "ACINETOBACTER INFECTION". Virginia Department of Health. 2018.
- ↑ Dijkshoorn, Lenie; Nemec, Alexandr; Seifert, Harald (2007). "An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii". Nature Reviews Microbiology. 5 (12): 939–951. doi:10.1038/nrmicro1789. ISSN 1740-1526. PMID 18007677. S2CID 3446152.
- ↑ Centers for Disease Control and Prevention (U.S.) (November 2019). "Antibiotic resistance threats in the United States, 2019". Antibiotic Resistance Threats in the United States. doi:10.15620/cdc:82532. S2CID 241621099.
- ↑ Falagas, M. E.; Kasiakou, S. K.; Saravolatz, L. D. (2005-05-01). "Colistin: The Revival of Polymyxins for the Management of Multidrug-Resistant Gram-Negative Bacterial Infections". Clinical Infectious Diseases. 40 (9): 1333–1341. doi:10.1086/429323. ISSN 1058-4838. PMID 15825037. S2CID 21679015.
- ↑ Falagas, Matthew E; Kasiakou, Sofia K (2006). "Toxicity of polymyxins: a systematic review of the evidence from old and recent studies". Critical Care. 10 (1): R27. doi:10.1186/cc3995. PMC 1550802. PMID 16507149.
- ↑ 13.0 13.1 Cheon, Shinhye; Kim, Mi-Ja; Yun, Seon-Jin; Moon, Jae Young; Kim, Yeon-Sook (2016-03-01). "Controlling endemic multidrug-resistant <i>Acinetobacter baumannii</i> in Intensive Care Units using antimicrobial stewardship and infection control". The Korean Journal of Internal Medicine. 31 (2): 367–374. doi:10.3904/kjim.2015.178. ISSN 1226-3303. PMC 4773730. PMID 26874513.