User:Mr. Ibrahem/Anthrax
| Anthrax | |
|---|---|
| Other names | Anthrax disease |
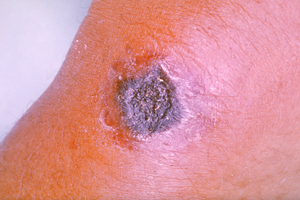 | |
| A skin lesion caused by anthrax; the characteristic black eschar | |
| Medical specialty | Infectious disease |
| Symptoms | Skin form: small blister with surrounding swelling Inhalational form: fever, chest pain, shortness of breath Intestinal form: nausea, vomiting, diarrhea, abdominal pain Injection form: fever, abscess[1] |
| Usual onset | 1 day to 2 months post contact[1] |
| Causes | Bacillus anthracis[2] |
| Risk factors | Working with animals, travelers, postal workers, military personnel[3] |
| Diagnostic method | Based on antibodies or toxin in the blood, microbial culture[4] |
| Prevention | Anthrax vaccination, antibiotics[3][5] |
| Treatment | Antibiotics, antitoxin[6] |
| Prognosis | 20–80% die without treatment[5][7] |
| Frequency | >2,000 cases per year[8] |
Anthrax is an infection caused by the bacterium Bacillus anthracis.[2] It can occur in four forms: skin, lungs, intestinal, and injection.[9] Symptom onset occurs between one day to over two months after the infection is contracted.[1] The skin form presents with a small blister with surrounding swelling that often turns into a painless ulcer with a black center.[1] The inhalation form presents with fever, chest pain, and shortness of breath.[1] The intestinal form presents with diarrhea which may contain blood, abdominal pains, nausea, and vomiting.[1] The injection form presents with fever and an abscess at the site of drug injection.[1]
Anthrax is spread by contact with the bacterium's spores, which often appear in infectious animal products.[10] Contact is by breathing, eating, or through an area of broken skin.[10] It does not typically spread directly between people.[10] Risk factors include people who work with animals or animal products, travelers, postal workers, and military personnel.[3] Diagnosis can be confirmed by finding antibodies or the toxin in the blood or by culture of a sample from the infected site.[4]
Anthrax vaccination is recommended for people who are at high risk of infection.[3] Immunizing animals against anthrax is recommended in areas where previous infections have occurred.[10] A two-months' course of antibiotics such as ciprofloxacin, levofloxacin, and doxycycline after exposure can also prevent infection.[5] If infection occurs, treatment is with antibiotics and possibly antitoxin.[6] The type and number of antibiotics used depends on the type of infection.[5] Antitoxin is recommended for those with widespread infection.[5]
Although a rare disease, human anthrax, when it does occur, is most common in Africa and central and southern Asia.[11] It also occurs more regularly in Southern Europe than elsewhere on the continent, and is uncommon in Northern Europe and North America.[12] Globally, at least 2,000 cases occur a year with about two cases a year in the United States.[8][13] Skin infections represent more than 95% of cases.[7] Without treatment, the risk of death from skin anthrax is 24%.[5] For intestinal infection, the risk of death is 25 to 75%, while respiratory anthrax has a mortality of 50 to 80%, even with treatment.[5][7] Until the 20th century, anthrax infections killed hundreds of thousands of people and animals each year.[14] Anthrax has been developed as a weapon by a number of countries.[7] In plant-eating animals, infection occurs when they eat or breathe in the spores while grazing.[11] Animals may become infected by eating infected animals.[11]
References
change- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 "Symptoms". CDC. 23 July 2014. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ↑ 2.0 2.1 "Basic Information What is anthrax?". CDC. 1 September 2015. Archived from the original on 17 May 2016. Retrieved 14 May 2016.
- ↑ 3.0 3.1 3.2 3.3 "Who Is at Risk". CDC. 1 September 2015. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ↑ 4.0 4.1 "Diagnosis". CDC. 1 September 2015. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Hendricks, KA; Wright, ME; Shadomy, SV; Bradley, JS; Morrow, MG; Pavia, AT; Rubinstein, E; Holty, JE; Messonnier, NE; Smith, TL; Pesik, N; Treadwell, TA; Bower, WA; Workgroup on Anthrax Clinical, Guidelines (February 2014). "Centers for disease control and prevention expert panel meetings on prevention and treatment of anthrax in adults". Emerging Infectious Diseases. 20 (2). doi:10.3201/eid2002.130687. PMC 3901462. PMID 24447897.
- ↑ 6.0 6.1 "Treatment". CDC. 14 January 2016. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ↑ 7.0 7.1 7.2 7.3 "Anthrax". FDA. 17 June 2015. Archived from the original on 7 May 2016. Retrieved 14 May 2016.
- ↑ 8.0 8.1 Anthrax: Global Status. GIDEON Informatics Inc. 2016. p. 12. ISBN 9781498808613. Archived from the original on 10 September 2017.
- ↑ "Types of Anthrax". CDC. 21 July 2014. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ↑ 10.0 10.1 10.2 10.3 "How People Are Infected". CDC. 1 September 2015. Archived from the original on 26 December 2016. Retrieved 14 May 2016.
- ↑ 11.0 11.1 11.2 Turnbull, Peter (2008). Anthrax in humans and animals (PDF) (4 ed.). Geneva, Switzerland: World Health Organization. pp. 20, 36. ISBN 9789241547536. Archived (PDF) from the original on 30 November 2016.
- ↑ Schlossberg, David (2008). Clinical Infectious Disease. Cambridge University Press. p. 897. ISBN 9781139576659. Archived from the original on 10 September 2017.
- ↑ "Anthrax". CDC. National Center for Emerging and Zoonotic Infectious Diseases. 26 August 2009. Archived from the original on 26 December 2016. Retrieved 14 May 2016.
- ↑ Cherkasskiy, B. L. (1999). "A national register of historic and contemporary anthrax foci". Journal of Applied Microbiology. 87 (2): 192–195. doi:10.1046/j.1365-2672.1999.00868.x. PMID 10475946. S2CID 6157235.